MESSAGE FROM THE DIRECTOR
- At AUBMC and with the Naef K. Basile Cancer Institute, we believe in caring for the whole person — not just the disease or symptom. Our comprehensive approach to medicine weaves into a cancer patient’s overall care plan, based on the latest scientific evidence.
- From boosting your overall sense of well-being to managing your pain, with experts trained in lymphedema therapy, the Physical Therapy Department offers specialized advice and a program that can help you manage lymphedema during the cancer journey.
- Disorders of the lymphatic system including lymphedema have a high incidence and represent a serious health issue for patients across different health conditions.
- Complete Decongestive Therapy which includes Manual Lymphatic Drainage as a core element has risen as a state-of-art management approach targeting lymphatic disorders and successfully managing them.
- Our program follows a pioneering comprehensive approach to the management of chronic diseases like cancer: reaching beyond the realm of managing treatment and side effects towards quality-of-life care.
- To prevent and treat lymphedema, from diagnosis to treatment and survivorship, our experts in lymphedema therapy provide the care and support you need, when you need it. We welcome outside patients seeking consultation.
LYMPHATIC DRAINAGE
- Lymphatic drainage is a manual massage method used to reduce swelling caused by lymphedema or lymph fluid buildup after cancer treatment.
- By gently manipulating specific areas of the body, this type of drainage helps move fluid from a swollen area to another where the lymphatic system is working normally.
- It is a light skin stretching manual pressure method that releases lymphatic fluid out of the swollen limb/extremity. It is used to relieve lymphedema which often affects:
• Women recovering from breast cancer treatment
• Women affected by lymphedema after hysterectomy for cervical cancer
• Men affected by prostate cancer
- Manual Lymphatic Drainage as a core component of Complete Decongestive Therapy alongside exercise, compression bandages, skin care, and breathing techniques targets the physiology of the lymphatic system through allowing decongestion of the affected region.
- The technique leads to opening of the functional lymph collectors to move fluid into them while speeding lymph flow through the limb.
OBJECTIVES OF LYMPHATIC DRAINAGE TREATMENT
- The intention behind Manual Lymphatic Drainage is to mimic the rhythmic contractions and stimulate the lymph nodes to improve their function and reroute stagnant lymphatic fluid.
- It is effective as a preventive and postoperative rehabilitation treatment. Manual Lymphatic Drainage also increases blood flow in deep and superficial veins.
- Manual Lymphatic Drainage may be useful in conditions such as post-traumatic and post-surgical edema and palliative care.
INDICATIONS FOR LYMPHATIC DRAINAGE IN CANCER
- MANUAL LYMPHATIC DRAINAGE can span throughout cancer survivorship: from diagnosis, treatment to post treatment management
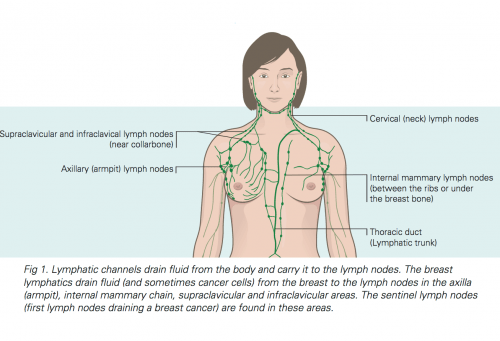
- It is indicated and is effective in tumor causing lymphatic obstruction of the anterior cervical, thoracic, axillary, breast, pelvic, prostatic or abdominal nodes such as in breast and prostate cancer.
- Lymphedema can occur after any cancer or its treatment that affects lymph node drainage. It can occur within days and up to 30 years after treatment for breast cancer.
- Upper-extremity lymphedema most often occurs after breast cancer; lower-extremity lymphedema most often occurs with uterine cancer, prostate cancer, lymphoma, or melanoma.

Prevention treatment of edema:
- Swelling at a limb’s root
- Leg edema during prostate cancer
- Leg edema after hysterectomy in cervical cancer
- Trunk and midline edema
- Arm and underarm edema in breast cancer
- Breast edema after breast reconstruction or mastectomy
Palliative treatment of edema:
- Palliative treatment adjunct to pain management: when comfort and pain relief are required but other therapies are no longer appropriate
When is lymphatic drainage massage indicated:
1. Loss of functional use of an upper or lower extremity limb due to edema size, weight, and loss of motion
2. Circumference measurements showing > 2cm difference between the affected and non-affected limb at 3 measured points along the extremity
3. Scar tissue formation that limits normal range of motion (ROM) and function, and disrupts normal lymphatic drainage
4. Palliative care pain relief, comfort and prevention of further functional loss of the affected limb
5. Loss of range of motion that limits a patient’s ability to obtain the proper radiation position
General contraindications:
Are there any risks associated with lymphatic drainage massage?
Generally, lymphatic drainage massage is a safe treatment to relieve lymphedema.
Some conditions where lymphatic drainage massage might not be advised:
- Cancer metastases
- Primary tumours
- Heart condition: Severe cardiac insufficiency
- Kidney failure
- Hepatic cirrhosis with abdominal fluid (ascites)
- Blood clots
- An infection
- Acute cellulitis/erysipelas
- Unstable hypertension
- Untreated tuberculosis or malaria
- Impaired arterial perfusion
- Superior vena cava obstruction
- Untreated thyroid dysfunction
- History of deep vein thrombosis and current use of anticoagulant medications
- History of diabetes mellitus
Consult your physician to make sure your health status allows lymphatic drainage.
Compression Bandages and Garments Contraindications:
1. Arterial disease and/or ulcers. An arterial Doppler or perfusion test can be used to rule them out.
a. Signs and symptoms of arterial disease include: diminished pulse compared to opposite extremity; pale, bluish, smooth, shiny and cold or clammy skin; and presence of arterial ulcers. Test for capillary refill in the nail beds.
b. Signs and symptoms of arterial ulcers: distal 1/3 of lower leg, small, round, shallow, little drainage, pain with elevation.
2. Signs of infection or wound
WHAT IS DONE IN LYMPHATIC DRAINAGE?
- Depending where your swelling is, you lie down or sit up.
- A specially trained therapist uses targeted skin movements to move fluid out of the swollen area and prepare the area the fluid will move to.
- Manual lymphatic drainage is very light to the touch. It begins on unaffected areas to direct the lymph away from the affected extremity. It decreases congestion of lymph nodes by directing lymph fluid it to the circulatory and lymphatic system.
- The therapist gently pressures the skin, with slow and rhythmic movements that help open lymph vessels and drain excess fluid.
- The number of sessions you have will depend on the state of your lymphedema.
- A lymphatic drainage massage is usually a two-step process:
- Clearing: This step releases lymphatic fluid in your tissues.
- Reabsorption: This step moves your lymphatic fluid to your lymph nodes.
- The therapist might bandage the area after the drainage session or might ask you to wear compression garments.
- Talk to your Dr. and therapist about any changes you notice or not in the state of your swelling.
DIFFERENT LYMPHATIC DRAINAGE APPROACHES
It is often given as part of Complete Decongestive Therapy which has two phases – phase I and II.
- Complete decongestive therapy
Complete decongestive therapy is a multimodality program that consists of manual lymphedema drainage therapy, low-stretch bandaging, exercises, and skin care. Complex decongestive therapy is divided into two successive phases. The first phase consists of intensive treatment to allow substantive reduction of lymphedema volume. The second phase consists of maintenance treatment at home. Compliance with the use of the elastic sleeve and low-stretch bandage has been found to be an important determinant of success with maintenance therapy at home.



- Manual Lymphatic Drainage is performed in phase I and II, but phase II involves more drainage. The two phases consist of the following:
Phase I
– MANUAL LYMPHATIC DRAINAGE
– Lymphological compression bandages
– Remedial exercises
– Traditional physiotherapy if patients are struggling with mobility or joint mobility/function impairments.
– Education regarding self-management and skin care
Phase II
– MANUAL LYMPHATIC DRAINAGE
– Wearing of fitted compression stockings
– Night Garments
Two drainage techniques are applied:
- Vodder: Different kinds of hand motions are used on the skin depending on the part of the body being treated. It also includes movements to handle edema at fibrotic areas. The different motion techniques include “pump”, “scoop”, “stationery circle”, “rotary” and “thumb circle”.
- Foldi: Based on the Vodder technique, this method lays emphasis on a “thrust” and “relaxation” phase. ‘Encircling strokes’ are included in this approach.
Exercise
Non fatiguing exercises may induce sufficient muscle contraction to move lymph into terminal lymphangioles and reduce swelling. Aerobic exercise may also increase the tone of the sympathetic nervous system, which causes the lymph collector vessels to pump more vigorously.
Gradient pressure garments
Gradient pressure garments (also known as lymphedema sleeves or stockings) generate greater pressures distally than proximally, which enhances mobilization of edema fluid. The use of these garments may be especially important at high altitudes, such as during air travel, because the ambient atmospheric pressure is less than the outlet transcapillary pressure within the superficial tissues, which can lead to worsening edema.
Bandages
Bandaging involves the use of inelastic material to discourage reaccumulation of lymph by reducing capillary ultrafiltration and optimizing the efficacy of the intrinsic muscle pump. Bandaging may change an initially resistant limb to one with less edema, resulting in decreased limb volume and allowing a garment to be applied successfully.
Skin care
The goal of skin care is to minimize dermal colonization by bacteria and fungus, especially in the crevices, and hydrate the skin to control dryness and cracking.
Frequency & Duration:
The frequency and duration may range from a onetime visit for an assessment and education regarding lymphedema prevention to 2-3 visits per week for 6 or more weeks depending on the severity of lymphedema and associated impairment.
LYMPHATIC treatment GOals
The goal of lymphedema treatment with complete decongestive therapy and lymphatic drainage is to control limb swelling and minimize complications, while the underlying lymphatic vessel interruption resulting from cancer surgery cannot be adressed.
Drainage aims to maximize the activities of daily living, decrease pain, increase a patient’s range of motion, and improve function. Short and long term goals to be met in 4-8 weeks may include but are not limited to:
1. Independence with home exercise program
2. Independence with compression bandaging
3. Independence with self massage techniques
4. Independence with lymphedema prevention and risk factor reduction strategies
5. Reduce limb circumference by 25-50%
6. Maximize range of motion
7. Maximize strength
8. Independence with postural correction in various positions
9. Maximize independence with functional activities
MEET OUR TEAM
The Lymphatic Drainage Program team relies on experts specifically educated, trained and experienced in each method, as the program involves Physiotherapist-Administered Manual Lymphatic Drainage.
Charbel Rizk, PT, DPT
Physical Therapy Department manager
01 350 000 Ext: 6645 6648
Dr. Rizk holds a master’s degree in physical and sports actvities and a doctorate degree in Physical Therapy from Saint Joseph University.
He is a dedicated Physical Therapist with over thirty years experience evaluating and effectively managing the treatment of patients. Dr. Rizk built his expertise track around accurately assessing the needs of patients, creating appropriate treatment plans and rehabilitation processes to best address their needs.
Dr. Rizk has been practicing physical therapy since 1991 at AUBMC and is currently the Physical Therapy department’s manager.
Colette Nassar, PT, DPT, CLT certified
Certified lymphedema therapist
01 350 000 Ext: 6648 6645
Dr. Nassar has been practicing physical therapy since 1991 at AUBMC.
She holds a Bachelor of Science in Physical Therapy from the Lebanese University and earned a master’s degree in Neurological Rehabilitation and a doctorate degree with honors in Physical Therapy from Saint Joseph University. Her doctorate research focused on stroke patients.
Dr. Nassar’s field of expertise is in rehabilitation of neurological cases such as strokes, developmental delay in children, orthopedic injuries, and spinal diseases (back and neck pain). Colette also has a wide experience in all domains of Physical Therapy.
In 2016, she specialized in clinical lymphatic draining from the Klose Institute in Chicago (in manual lymph drainage (Vodder technique), complete decongestive therapy and lymphedema bandaging), and is a Clinical Lymphatic Trainer (CLT). Dr. Nassar introduced this method to AUBMC, which is mainly applied to patients with lymphatic and oedema issues resulting from breast cancer and surgeries.
Dr. Nassar is always aspired to learn more and gain more experience to further her field of knowledge and work, and help patients with her expertise and skills.
LOCATION AND APPOINTMENT SCHEDULING
The newly established LYMPHATIC CARE PROGRAM welcomes patients with lymphedema. Consult with your NKBCI physician for recommended treatments.
To schedule an appointment with one of the specialists, kindly contact the physical therapy department on 01-315 000, Ext. 6645 or 6648.
- Location: AUBMC, Phase 1 Building, 3rd floor
- Date and Time: Weekdays from 7.30am till 5 pm
- The first visit will last about 45 minutes and will consist of a physical evaluation based on the physician’s prescription.
- The therapist will tailor an individualized physical therapy plan of treatment that considers your physical condition and lifestyle demands, to prepare you to return to your highest possible functional level at home, work and leisure.
- Follow-up visits will last from 30 minutes to 45 minutes depending on your treatment plan.
Reach Us Directly!
What is Lymhadema
Introduction
- Lymphedema is swelling that occurs when protein-rich lymph fluid accumulates in the interstitial tissue. This lymph fluid may contain plasma proteins, extra vascular blood cells, excess water, and parenchymal products.
- Over time, it can lead to fibrosis or hardening of the dermal tissue, chronic inflammatory reactions and poor healing.
- The most common type of lymphedema is secondary, or acquired, lymphedema, which is caused as a result of tumor, trauma, chronic venous insufficiency and treatment for medical conditions, most notably for breast cancer and other malignancies.
- Lymphedema may develop in an extremity, the breast, and/or in the face, neck or trunk as a result of damage to the lymphatic transport system in an adjacent part of the body.
Anatomy and Pathophysiology of the Lymphatic System
- The human lymphatic system generally includes superficial or primary lymphatic vessels that form a complex dermal network of capillary like channels that drain into larger, secondary lymphatic vessels located in the subdermal space.
- One function of the lymphatic system is to return excess fluid and protein from interstitial spaces to the blood vascular system. Because lymphatic vessels often lack a basement membrane, they can resorb molecules too large for venous uptake.
- Mechanisms of clinical edema include increased arteriovenous capillary filtration and reduced interstitial fluid absorption. Causes of increased capillary filtration include increased hydrostatic pressure in capillaries, decreased tissue pressure, and increased membrane permeability.
- Reduced interstitial fluid resorption can be caused by decreased plasma oncotic pressure, increased oncotic pressure of tissue fluid, and lymphatic obstruction.

Symptoms of Lymphedema
How is lymphedema diagnosed?
Your physician will perform a physical exam and take your medical history, checking about:
- Past surgeries
- Any problems after surgeries
- When the swelling started
- History of swelling (edema)
- Medications you are taking
- Other health conditions : such as high blood pressure, heart disease, or diabetes
Imaging tests, measures of volume, blood tests, and other tests may be used to diagnose lymphedema.
Lymphadema stages
Stage I is spontaneously reversible and typically is marked by pitting edema, increase in upper-extremity girth, and heaviness.
Stage II is characterized by a spongy consistency of the tissue without signs of pitting edema. Tissue fibrosis can then cause the limbs to harden and increase in size.
Stage III, also called lymphostatic elephantiasis, is the most advanced stage, but is rarely seen following breast cancer treatment.
Risk factors for lymphadema
Patients undergoing axillary surgery and/or axillary radiation therapy for breast cancer are at higher risk for developing lymphedema of the arm. Previous convention suggested that nodal positivity was a predisposing factor for the development of lymphedema in breast cancer patients.
1. Axillary node removal
Compared with axillary sampling alone, partial or total mastectomy followed by full axillary lymph node dissection significantly increases a patient’s chance of developing arm edema.
2. Obesity
Among all breast cancer patients, being obese or overweight may predispose women to developing lymphedema after treatment for breast cancer.
3. Other risks
Other risk factors for developing lymphedema include the following:
· Extent of local surgery.
· Local radiation (axillary, inguinal, pelvic, or supraclavicular regions).
· Delayed wound healing.
· Tumor causing lymphatic obstruction of the anterior cervical, thoracic, axillary, pelvic, or abdominal nodes.
· Scarring of the left or right subclavian lymphatic ducts by either surgery or radiation.
· Intrapelvic or intra-abdominal tumors that involve or directly compress lymphatic vessels and/or the cisterna chyli and thoracic duct.
Treatment for Lymphedema
Treatment includes approaches to prevent and manage the condition, and may include:
-
- Lymphatic drainage: Manual to release trapped fluid out of swollen area.
-
Complete decongestive therapy: a multimodality program that consists of manual lymphedema drainage therapy, low-stretch bandaging, exercises, and skin care.
- Exercise: Helps you heal properly and regain strength. Using your muscles also helps the lymph fluid circulate and drain like it should. It also helps keep your muscles flexible and helps reduce scarring. Specific exercises will be advised by your doctor or physical therapist. Non fatiguing exercises may induce sufficient muscle contraction to move lymph into terminal lymphangioles and reduce swelling. Aerobic exercise may also increase the tone of the sympathetic nervous system, which causes the lymph collector vessels to pump more vigorously.
- Bandages: Wearing a compression sleeve or elastic bandage may help to move fluid and prevent the buildup of fluid.
- Compression garments: Close-fitting elastic sleeves or stockings can compress the arm or leg to encourage lymph fluid drainage.
- Diet and weight management: A healthy diet and controlling body weight is an important part of treatment. Being obese puts people at higher risk for lymphedema
- Keeping the arm raised: Raising the arm above the level of the heart when possible, lets gravity help drain the fluid.
- Preventing infection: It’s important to protect the skin in the affected area from drying, cracking, infection and skin breakdown. Your physician will advise you about how to care for your skin and nails to help prevent problems.
- Elevating affected areas: Whenever you can, keep your affected arm or leg lifted above your heart.
Can lymphedema be prevented?
- There is no sure way to prevent lymphedema. If you’re experiencing lymphedema after breast cancer surgery and radiation therapy, or with prostate or cervcal cancer, the experts at Naef K. Basile Cancer Institute recommend prompt treatment. For many patients, lymphedema therapy can be extremely helpful. It’s important to note that there is no known cure for lymphedema at this time. However, the approaches described here may help ease symptoms.
- Newer types of lymph node surgery have also helped decrease lymphedema risk. But there is no sure way to prevent lymphedema.
- Women and men treated for cancer who exercise after treatment are less likely to develop lymphedema.
- Exercise helps improve the effect of lymph drainage. Specific exercises will be advised by your doctor or physical therapist.
Lymphedema during breast cancer
- Lymphedema happens when tissues retain the fluid left behind after the heart sends blood to your tissues and organs.
- The remaining fluid is called lymph. Normally, the lymphatic system collects lymph and returns it to the heart via lymph vessels and lymph nodes. When this process is disrupted, lymph collects in your arms and legs, making them swell.
- In breast cancer surgery, the removal of lymph nodes can disrupt the lymph’s regular flow, which can lead to swelling and lymphedema. It usually affects the arm on the side where lymph nodes have been removed.
- Lymphedema can affect one or both arms, the head and neck, the belly, the genitals, or the legs. Swelling can worsen and become severe.
- Radiotherapy that also targets lymph nodes under the arm -which drain lymphatic vessels from upper arms, the breasts, chest, neck and underarm area- can cause scarring and blockages that further increase the risk of lymphedema.
- When a number of lymph nodes under the arm have been removed, a woman is at a higher risk of lymphedema.
- Lymphedema may occur right after surgery or radiation, or months or even years later.
Preventing Infection and Injury in lymphedema
Education
Ideally, prevention should begin before treatment, by educating the patient and family in a sensitive fashion about the potential risk of developing lymphedema. Patients should be taught to recognize the early signs of edema because treatment outcomes may be significantly improved if the problem is detected early.
Hygiene: Skin and Nail Care
Lymphedema and poor drainage of the lymphatic system puts stress on your skin, making it more vulnerable to infection from injuries like cuts, scrapes and scratches and less sensitive to extreme temperature.
Be aware of activities that put too much pressure on the affected arm.
To protect your arm from injury and infection, make sure to do the following:
- Clean the skin of the affected arm daily
- Wash your hands regularly: throughout the day, before preparing food and after going to the bathroom or touching dirty clothes or linens.
- Moisturise the skin daily to keep it supple with a suitable cream
- Use skin moisturizers and topical antibiotic solutions after small breaks in the skin, such as paper cuts.
- Wear gardening and cooking gloves and use thimbles for sewing.
- Treat any cuts and scratches immediately: with soap and water and an antiseptic, apply antibiotic ointment and put a bandage on your injury.
- Avoid going barefoot outdoors.
- Avoid blood draws (including finger sticks), vaccinations, or intravenous lines in the affected arm.
- Ask for all blood pressure tests to be done on the unaffected arm.
- Avoid tight or restrictive clothing or jewelry: can squeeze the arm or leg unevenly or too much, which might increase the pressure in nearby blood and lymph vessels. Make sure your watch or jewelry isn’t squeezing your arm.
- Wear sun protection (SPF 30 or higher) to prevent sunburn to affected areas.
- Wear insect repellent to avoid bug bites that could make you want to scratch.
- Wear cotton socks; keep feet clean and dry: Avoid tight-fitting socks, tights and hosiery and wear comfortable, closed-toe shoes.
- Don’t wear nightgowns or clothing with elastic cuffs or tight bands.
- Use the unaffected extremity to test temperatures (e.g., for bath water or cooking), as sensation may be diminished.
- Carry your handbag or heavy packages with the unaffected arm.
- Prefer using an electric razor when you shave.
- Do approved exercises regularly to improve drainage.
- Avoid very hot baths and showers – the heat from saunas, steam rooms and sun beds, heating padsmay increase the swelling or cold temperatures or ice packs.
- Cut toenails straight across; see a podiatrist as needed to prevent ingrown nails and infections. Don’t cut or bite your cuticles.
- Avoid vigorous, repetitive movements, such as scrubbing, pulling, or pushing with the affected arm.
- Be aware of the signs of infection (fever, swelling, redness, pain, and heat) and see a physician for evaluation immediately.
Tell your doctor right away if you have any signs of infection, such as redness, pain, heat, increased swelling, or fever.
Extremity Positioning
· Keep the arm or leg elevated above the level of the heart when possible.
· Avoid constrictive pressure on the affected arm or leg.
– Do not cross legs while sitting.
– Wear loose jewelry and clothes with no constricting bands.
– Carry a handbag on the opposite arm.
– Do not use elastic bandages and stockings with constrictive bands.
– Do not sit in one position for longer than 30 minutes.
– Do not sleep over the affected limb
Avoiding the Pooling of Blood in the Involved Extremity
· Avoid rapid circular movements that cause centrifugal pooling of fluid in distal parts of the limb.
· Avoid local application of heat to the limb, which may increase blood flow.
· Do not maintain the limb in a gravity-dependent position for long periods of time.
· Avoid tight-fitting clothing or blood pressure monitoring in the affected arm, which could cause a tourniquet effect and obstruct lymph flow.
How does exercise help with lymphedema?
- Exercise is one of the best ways to keep fluid moving. Talk to your physician before starting an exercise routine. He will have suggestions and may recommend special exercises you can do. Other suggestions are:
-
- Warm-up and cool down: No matter your routine, start with a five-minute warm-up of stretches and end with a five- to 10-minute cool down.
- Take it slow: Give your body time to adjust to your exercise routine. Start with 10 minutes of exercise, with a goal of doing 20 to 30 minutes of exercise each day.
- Take it easy: Avoid strenuous exercise that puts pressure on your affected arm or leg.
- Wait on weights: If you normally lift weights or do strength training, ask your healthcare provider when you can resume training. They may have suggestions on exercises you should avoid or limits on the amount of weight you should lift.
- Don’t push yourself: Pay attention to your affected arm or leg and take a break if you notice your arm or leg begins to weaken. Do your cool-down routine and then rest your arm or leg, elevating it above your heart.
- Don’t push through pain: Stop any exercise that hurts and contact your provider. They may want to check your affected arm or leg.
How does Diet Help?
Healthy eating habits may help control swelling. Your lymphatic system is more effective when it’s well nurtured with healthy nutrients from from fruits, vegetables, whole grains and lean protein. Healthy eating also helps you maintain a weight that’s right for you.
Some suggestions include:
- Pass (on) the salt: Salt can make you retain fluids. Try fresh herbs and other seasonings to spice up your food.
- Drink your water: Drinking eight 8-ounce glasses of water every day helps flush out fluids.
QUICK LINKS


